Future Focus: Jameson Trainor
 Jameson Trainor was one of the five recipients to receive our FutureFocus grant for 2019, and at the time was a second year medical student from the University of Melbourne. Jameson received $2 500 to put towards his overseas voluntary placement in Ghizo, Solomon Islands. His placement involved working in Gizo Hospital specifically in the Accident and Emergency department.
Jameson Trainor was one of the five recipients to receive our FutureFocus grant for 2019, and at the time was a second year medical student from the University of Melbourne. Jameson received $2 500 to put towards his overseas voluntary placement in Ghizo, Solomon Islands. His placement involved working in Gizo Hospital specifically in the Accident and Emergency department.
Read a full account from Jameson about his incredible journey below.
Elective reflection
I was fortunate enough to spend four weeks in the Solomon Islands undertaking a Medical elective at Gizo Hospital. This placement highlighted to me how fortunate we are in Australia with relatively easy access to highly specialised healthcare.

Gizo Hospital is set on Ghizo Island in the Western Province of the Solomon Islands. It is the main hospital in the province and the second largest hospital in the country, only to the National Referral Hospital in the capital, Honiara. The Solomon’s health network is set up with nurse aid posts, rural and area health clinics and provincial hospitals. Access to health care is a major problem for the Solomon people. I saw patients that had travelled for days to receive basic treatment. As it is the Solomon Islands, almost all travel is by small banana shaped boats. Even getting to the town from the airport was via one of these boats! All patients from outside of town, emergency or otherwise, didn’t come by an ambulance but rather by one of these small wooden boats. This provided a unique challenge for patients’ access to healthcare that we don’t see in Victoria.
Whilst being the second largest hospital in the country, Gizo Hospital does not have the same equipment as many Melbourne hospitals have. The hospital radiology department had two X-ray machines, one being portable and two ultrasound machines. There was no CT in the hospital or at the National Referral Hospital. This proved to be challenging when an elderly man presented to the ED with a sudden onset left lower limb paralysis. With a quick history and examination, it was clear this man was having a stroke. I asked my supervising Doctor how we were going to treat him, given there was no CT to further investigate the cause of problem. “Fluids and supportive treatment” was his answer. We could not do anything as we could not work out if it was a haemorrhagic or an ischaemic stroke. This was quite a shock to me. Having seen a few code ‘stroke’ calls at the St Vincent’s Hospital Melbourne ED, the timely management of a stroke was something that I took for granted. This was one of many examples of the differences in healthcare.
Despite these limitations the hospital did a fantastic job of caring for its patients. The hospital has an ED, two male, two female, two children, two post-natal wards, one labour and one TB ward. It also had two nursing and one doctors outpatient clinics, a non-communicable diseases clinic, physiotherapy and dental clinics.
The doctors did a fantastic job, often wearing multiple hats all in the one day (such as ED registrar, surgeon, anaesthetist, obstetrician, general practitioner). Whilst I was there, the three doctors provided a 24 hr on-call service amongst the general hospital duties during the day. Whilst I was mainly placed in the ED, I was able to experience all areas of healthcare that the hospital had to offer. I too, got to ‘wear many hats’, spending time interpreting X-rays, doing ultrasounds, seeing the pathology lab in action, doing post-natal ward rounds, seeing deliveries, seeing dental surgeries, assisting with surgical procedures, and seeing outpatients. I appreciated the opportunity to be involved in almost everything at the hospital and to be able to learn broadly.
I came into this elective with three main goals:
- To improve my clinical skills, such as managing patients from different cultures, enhancing my history taking and examination skills (given there is little medical technology available to rely on) and further refine my procedural skills.
- To compare hospital practices to my current placement at St Vincent’s Hospital Melbourne, learning to work with limited resources, not being wasteful or reliant on advanced clinical investigations.
- To be able to contribute to the medical services by taking over fundamental supplies for the hospital, providing my skills and experience whilst I was over there, as well as coming back and volunteering as a qualified doctor.
I was able to practice my history, examination and procedural skills. I did find history taking to be somewhat challenging due to a greater language barrier than I anticipated as well as with some patients being timid (both to myself and other local medical staff). This helped me appreciate the utmost importance of strong communication to be a good doctor.
I believe I was able to take away the most in comparing hospital practices and seeing the unique challenges of working in a resource poor setting. Whilst I cannot put it all into words, I saw medicine in a very different perspective. The most interesting experience that highlighted these challenges was when treating a 12-year-old girl who presented with a four day history of ascending paralysis, thought to be Guillain-Barré Syndrome (GBS). We did not have access to a ventilator which would be standard treatment of GBS in Australia. When the respiratory muscles are compromised and despite our best efforts to manually ventilate her, she passed away just 12 hours after we had first seen her in the ED. This was a significant moment for me, not only was it the first time I had experienced a patient die who I was helping treat, it was that had she been in Australia, this would have been a completely different scenario with a ventilator and ICU support managing the transient paralysis of GBS.
 I am glad that I was able to bring over some donations to give to the hospital. I would like to thank Laerdal Australia who kindly donated two CPR manikins, BOQ Specialist for their help in providing $500 for accessories to ensure the longevity of the manikins and MUHI Material Aid Program for their help in collecting various donations for the hospital. The staff were very appreciative of the donations and in particular were very excited to be able to practice scenarios with the manikins and improve their resuscitation skills.
I am glad that I was able to bring over some donations to give to the hospital. I would like to thank Laerdal Australia who kindly donated two CPR manikins, BOQ Specialist for their help in providing $500 for accessories to ensure the longevity of the manikins and MUHI Material Aid Program for their help in collecting various donations for the hospital. The staff were very appreciative of the donations and in particular were very excited to be able to practice scenarios with the manikins and improve their resuscitation skills.

Whilst I was there the local government was hosting the Western Provincial Cup, a sporting tournament of teams from around the province in soccer, netball, volleyball and boxing. I was lucky to join the team, with one of the ED nurses and one of the physios to watch some of the soccer matches as the medical team. I also teamed up with Dr Simbe to do a pre-bout medical check of all the boxers and then be ring side as a part of the medical team. It was a great experience watching the boxing, and during the second night there was a knockout that I attended to. In classic island time, the Doctor who I was with arrived 15 minutes after the knockout had happened so I was managing the patient by myself. Fortunately, he was ok. This was a very interesting experience for me, seeing the local and wider communities engage and support their respective teams and athletes, as well as having the chance to gain further experience in sports and pre-hospital medicine.

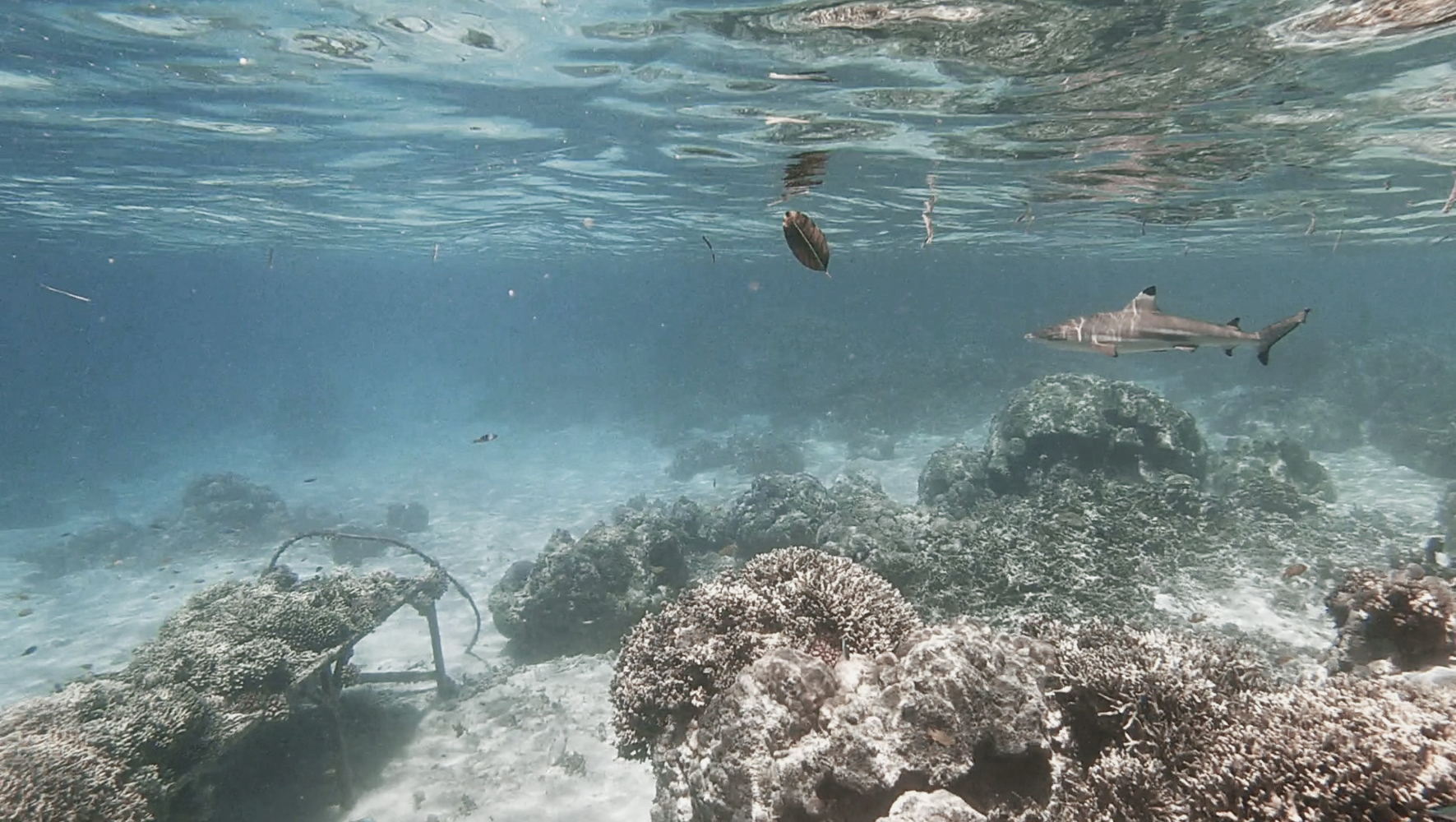 During my time away from the hospital I got the opportunity to explore some of the beautiful scenery the local Gizo area had to offer. Some highlights include going for a surf with Mizo (a Japanese nurse volunteering at the hospital) and some of the local surfers, snorkelling and seeing hundreds of different fish, exploring uninhabited islands and swimming with sharks (no cages involved!).
During my time away from the hospital I got the opportunity to explore some of the beautiful scenery the local Gizo area had to offer. Some highlights include going for a surf with Mizo (a Japanese nurse volunteering at the hospital) and some of the local surfers, snorkelling and seeing hundreds of different fish, exploring uninhabited islands and swimming with sharks (no cages involved!).
Summary
This elective has made me much more aware of how important basic healthcare is and it has shown me a very different perspective to medicine. For this, I am thankful. I plan to pursue further placements abroad to help broaden my scope of knowledge and experience. I would also like to take the opportunity to thank BOQ Specialist for their support in allowing me to undertake this incredible experience. I do think this elective has taught me many things that I would not have learnt otherwise in medical school and I would strongly encourage others to pursue similar experiences, to see how different medicine can be.
 Facebook
Facebook
Like and follow us on Facebook to keep up to date with all our student offers, events, competitions and more.